Measles in Maryland – Part I
This is the first of a series of articles on the U.S. measles outbreak of 2019. This installment will focus on Maryland modifications to measles recommendations, in light of the outbreak, and discuss the scale, sourcing, and spread that has precipitated the resurgence of a disease declared eliminated in 2000.
Later articles will focus on clinical guidance, provide resources for patient vaccine reticence, and give ongoing updates on the outbreak. We are asking physicians to share their strategies for talking to patients about the importance of vaccination and their go-to patient education materials, for future articles. Please send them to us by email or fax (301.921.4368.)
Maryland Modifications to the CDC’s Routine Measles Recommendations
MCMS asks all physicians to read the Maryland Department of Health’s (MDH) latest letter to clinicians which contains updated recommendations about measles vaccinations in special situations, and emphasizes important guidance for clinicians who might encounter patients exposed to measles or with suspected measles. This includes modifications to the CDC’s routine recommendations for patients who might be at increased risk of measles exposure. The measles outbreak in Maryland is currently localized to zip codes 21208, 21209 and 21215. Please check the MDH website health.maryland.gov/measles for the most up-to-date information on the outbreak.
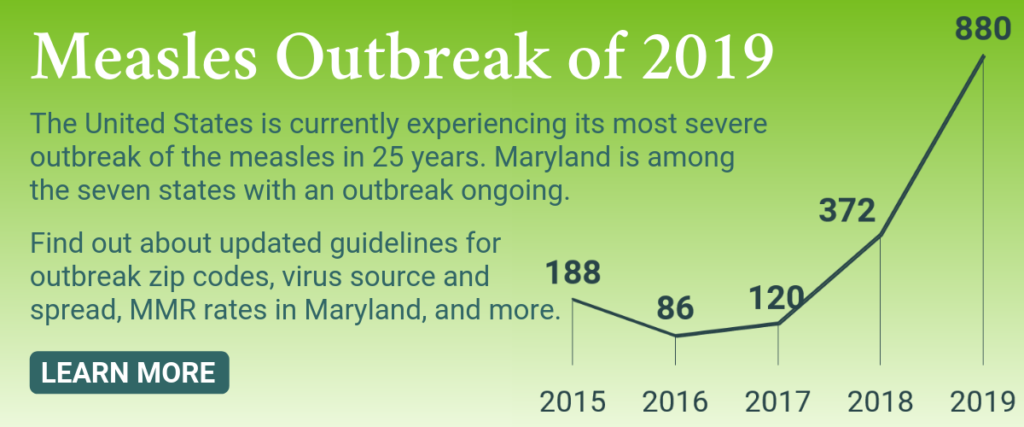
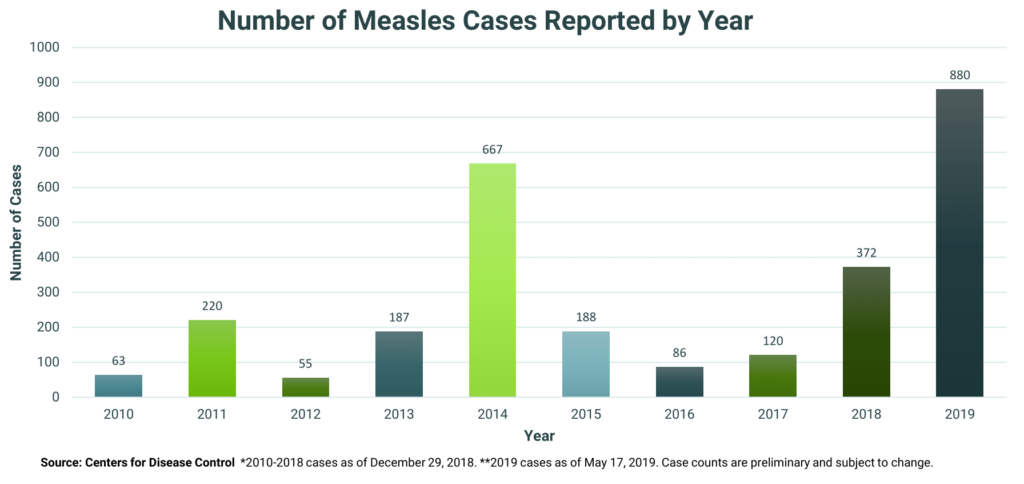
Largest Outbreak in 25 Years
Measles outbreaks (defined as 3 or more cases) are ongoing, as of May 23, 2019, in Maryland, New York, Michigan, California, Georgia, Pennsylvania, and Washington.
According to the CDC, from January 1 to May 17, 2019, 880 individual cases of measles have been confirmed in 24 states, an increase of 41 cases from the previous week. This is the greatest number of cases reported in the U.S. since 1994.
What Caused the Outbreak?
Initial outbreak reports are linked to travelers who brought measles back from other countries such as Israel, Ukraine, and the Philippines, where large measles outbreaks are occurring. According to the World Health Organization, the measles was responsible for 110,000 deaths in 2017 alone, making it one of the world’s most dangerous contagious diseases. In November of 2018, the WHO released a report indicating that measles would continue to spike globally due to gaps in vaccination coverage. Global reported cases of measles increased by more than 30 percent worldwide from 2016 to 2017.
The resurgence of measles is of serious concern, with extended outbreaks occurring across regions, and particularly in countries that had achieved, or were close to achieving measles elimination. Without urgent efforts to increase vaccination coverage and identify populations with unacceptable levels of under-, or unimmunized children, we risk losing decades of progress in protecting children and communities against this devastating, but entirely preventable disease.
Soumya Swaminathan, M.D., Deputy Director General for Programmes at WHO
Maryland Doesn’t Meet Measles Community Immunity Threshold
In Maryland, exemptions from vaccines can be made for religious reasons, though not for philosophical ones. The Community Immunity Thresholds (CIT) – the amount of vaccinated people needed to maintain community immunity – for the Measles, Mumps, and Rubella (MMR) vaccine is 95% for measles, 87% for mumps, and 86% for rubella.
As of 2017, the most recent data available, 92.4% of children 19-35 months old in Maryland have received the MMR vaccine (≥1 dose). The National Immunization Survey of 2017 estimated the same vaccination rate – 92.4% – for adolescents 13-17 years old (≥2 doses.) This means that the threshold for mumps and rubella community immunity are met, but not the threshold for measles. It’s also important to note that, while the CIT is within striking distance for immunity in Maryland, Washington D.C. lags far behind. Only 81% of kindergartners in DC have received the MMR vaccine. To learn more about child vaccination rates in Maryland, and how our state compares to national rates, visit the American Academy of Pediatrics or the CDC’s National Immunization Survey Dashboard.
Predictors of Low Vaccination Rates
The best predictors for whether or not a child aged 19 to 35 months has received at least one dose of an MMR are insurance coverage status and family mobility, more so than poverty line metrics, race, or ethnicity. According to the CDC, 75% of uninsured children in this group had received a dose of MMR, as opposed to 94% of privately insured children and 90% on Medicaid. A study from the CDC in 2016 noted that children who are up to date on their vaccinations, per clinical guidelines, tend to “live in households with fewer children, higher incomes and less mobility, compared to children who were not.” For more on predictors, visit this NPR article.
Resources & Further Reading:
- Maryland Department of Health’s Measles Resource Center
- “The Other Reasons Kids Aren’t Getting Vaccinations: Poverty And Health Care Access” from NPR
- “Viewpoints: Wiping Out Measles Again Means Focusing on Parent in Developing Countries” from Bloomberg
- “How Public Health Outreach Ended A 1990s Measles Outbreak and What’s Different Now” from NPR
- “Rare and Eradicated Diseases Making a Resurgence in the U.S.” from The DO
- “Mumps: The Disease, The Vaccine, The Problem” from the 2 Docs Talk Podcast
Key References:
- “Measles | Cases and Outbreaks | CDC.” Centers for Disease Control and Prevention. May 17, 2019.
- “Measles Cases Spike Globally Due to Gaps in Vaccination Coverage.” World Health Organization. November 29, 2018.
- “Child Vaccination Across America.” AAP.org. January 1, 2019.
