Smoking Cessation during COVID-19: Use Trends and Opportunities
Tobacco cessation has long been a key public health aim. It can only be considered more critical now during the pandemic, as smoking has long been known to hamper immune system responses, especially with regards to pulmonary diseases and infections.
With calls to quitlines down 27% in 2020, we must ask: How has COVID-19 impacted rates of smoking in the U.S. and what are its implications for patient care?
This article will present an overview of available statistics for smoking and vaping rates during the pandemic, provide references to the latest literature reviews on the risk factor severity of smoking on COVID-19, and provide practice resources for billing, patient education, clinical workflows, EHR integration, and more.
Smoking & Vaping Rates during COVID-19
Data for smoking and vaping rates during 2020 and the first quarter of 2021 is mixed and much of it is still preliminary.
As previously referenced, the North American Quitline Consortium reported on March 12, 2021 that just 525,000 calls were made to state quitlines during 2020, a 27% decrease from 2019 numbers and the lowest reported level since 2007. The drop in calls to state quitlines mirrored the timeline of the pandemic, with a 6% decrease in the first quarter of 2020, followed by decreases of 39%, 30%, and 21% in quarters two, three, and four respectively, compared to 2019. In 2019, just under one-third of callers were Medicaid enrollees and nearly half reported a co-occurring behavioral health condition such as depression or addiction.
National cigarette consumption rates, tracked monthly by the Alcohol and Tobacco Tax and Trade Bureau, echo this trend. After decreasing by 4-5% annually since 2015, cigarette sales increased 1% during 2020 compared to 2019.
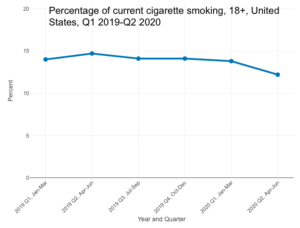
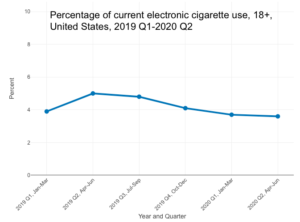
While the CDC’s National Health Interview Survey (NHIS), widely considered a standard for smoking and vaping statistics in the US, publishes data on a 30-month delay, there is some advance preliminary data available through their interactive data query system. This preliminary data generally conflicts with the above statistics, showing a modest decline in smoking and vaping during the first two quarters of 2020.
The early release table for current cigarette smoking for adults aged 18 and over shows a downtrend for 2020, from a rate of 14.1% in the fourth quarter of 2019 to 13.8% in the first quarter of 2020, and then another drop to 12.2% in the second quarter of 2020. The electronic cigarette and vaping early release table similarly reports a downtrend, from 4.1% in the fourth quarter of 2019, to 3.7% in the first quarter of 2020 and 3.6% in the second quarter of 2020.
Notably, e-cigarette unit sales analysis published by the CDC on September 18, 2020 suggested that the modest “decline in total e-cigarettes sales during August 2019–February 2020 might be attributable, in part, to shifts in consumer behaviors following the national outbreak of e-cigarette, or vaping, product use-associated lung injury”. Volumes began to bounce back after February 2020, as shown in the following unit sales graph from the same report.
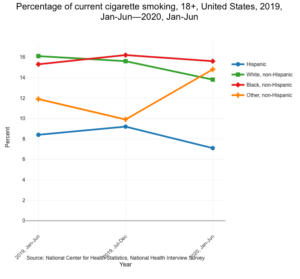
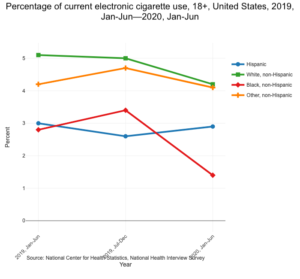
NHIS Biannual Estimates for the Total US Adult Population with a Focus on Demographic Subgroups documented differences in cigarette and e-cigarette use between white, non-hispanic, hispanic, black, non-hispanic, and other non-hispanic demographic groups, as shown below.
A recent article, “Changes in Tobacco Use During the 2020 COVID-19 Lockdown in New Zealand“, published in Nicotine & Tobacco Research on January 30, 2021 may help to bridge some of the data discrepancies shown above. The examination of self-reported smoking before and during the lockdown, suggested that while average nationwide statistics of the percentage of adults who smoke may remain stable, cigarette consumption by existing smokers may increase. Nearly half of daily smokers in the study “reported smoking more during than before the lockdown, on average, an increase of six cigarettes a day.”
Smoking and Severe COVID-19
The CDC science brief for Underlying Medical Conditions Associated with High Risk for Severe COVID-19 lists currently smoking or previously smoking as a high-risk factor for severe COVID-19, as does the WHO. The CDC’s science brief lists meta-analyses and systematic reviews which found a significant association with severe COVID-19. Those eight articles are linked below, in the order listed by the CDC. Notably, the CDC has not added to the smoking references list since the third quarter of 2020. Additional literature reviews from the fourth quarter of 2020 through the publishing date of this article are included in a separate list below.
CDC Science Brief References
- Zheng, Z., et al., Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect, 2020. 81(2): p. e16-e25. doi: 10.1016/j.jinf.2020.04.021
- Patanavanich, R. and S.A. Glantz, Smoking Is Associated With COVID-19 Progression: A Meta-analysis. Nicotine Tob Res, 2020. 22(9): p. 1653-1656. doi: 10.1093/ntr/ntaa082
- Guo, F.R., Active smoking is associated with severity of coronavirus disease 2019 (COVID-19): An update of a meta-analysis. Tob Induc Dis, 2020. 18: p. 37. doi: 10.18332/tid/121915
- Zhao, Q., et al., The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J Med Virol, 2020. 92(10): p. 1915-1921. doi: 10.1002/jmv.25889
- Lippi, G. and B.M. Henry, Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med, 2020. 75: p. 107-108. doi: 10.1016/j.ejim.2020.03.014
- Alqahtani, J.S., et al., Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS One, 2020. 15(5): p. e0233147. doi: 10.1371/journal.pone.0233147
- Li, J., et al., Meta-analysis investigating the relationship between clinical features, outcomes, and severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia. Am J Infect Control, 2020. doi: 10.1016/j.ajic.2020.06.008
- Farsalinos, K., et al., Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis. Ther Adv Chronic Dis, 2020. 11: p. 2040622320935765. doi: 10.1177/2040622320935765
Other Literature Reviews – September 2020-Present
- Askin Gülsen, Burcu Arpinar Yigitbas, Berat Uslu, Daniel Drömann, Oguz Kilinc, “The Effect of Smoking on COVID-19 Symptom Severity: Systematic Review and Meta-Analysis“, Pulmonary Medicine, vol. 2020, Article ID 7590207, 11 pages, 2020. doi.org/10.1155/2020/7590207.
- Gupta AK, Nethan ST, Mehrotra R. Tobacco use as a well-recognized cause of severe COVID-19 manifestations. Respiratory Medicine. 2021;176:106233. doi:10.1016/j.rmed.2020.106233.
- Rodgers, Aoife & Nadkarni, Manasi & Indreberg, Emilie & Alfallaj, Lenah & Kabir, Zubair. (2021). Smoking and COVID-19: A Literature Review of Cohort Studies in Non-Chinese Population Settings. Tobacco Use Insights. 14. doi.org/10.1177/1179173X20988671.
- Zhang, H., Ma, S., Han, T., Qu, G., Cheng, C., Uy, J. P., Shaikh, M. B., Zhou, Q., Song, E. J., & Sun, C. (2021). Association of smoking history with severe and critical outcomes in COVID-19 patients: A systemic review and meta-analysis. European journal of integrative medicine, 43, 101313. doi.org/10.1016/j.eujim.2021.101313.
- WHO Smoking & COVID-19 Scientific Brief
Smoking & Vaping Cessation: Resources for Medical Practices
Billing & Coding for Smoking Cessation
Two key codes for smoking cessation referenced in MCMS’s 2021 E&M Coding Updates Webinar:
- 99406 Smoking and tobacco use cessation counseling visit; intermediate, greater than three minutes up to 10 minutes
- 99407 intensive, greater than 10 minutes
Note: These codes are typically billed by internal medicine and family practice physicians who assume full care for smoking cessation as additional documentation is required. To bill 99406, specific methods for behavioral intervention must be addressed and documented to avoid relapse. This may also include prescribing pharmaceuticals or referrals to support groups. For 99407, the physician may include motivational interviewing techniques to address the positives and negatives for tobacco cessation. Additional therapies may be prescribed including nicotine replacement, pharmacologic adjuncts, support groups or a combination.
- AAFP Tobacco Cessation Telehealth Guide
- AAFP Guide: Integrating Tobacco Cessation Into Electronic Health Records
- AMA Behavioral Health Billing & Coding 101: How to Get Paid
- ALA Cessation Billing Guide
Patient Education Materials
- WHO COVID-19 & Tobacco Q&A – Includes information on vaping & COVID-19
- QuitNowTXT Message Library – Overview – PDF & Message Library – Excel
- Patient Handout: Help for Smokers and Other Tobacco Users – English, Spanish
- Patient Handout: Support and Advice From Your Prenatal Care Provider
- Patient Handout: You Can Quit Smoking
- 1-800-QUIT-NOW Cards
- Free Smoking & Tobacco Use Publications from the CDC
- Tips from Former Smokers
- Kick the Habit from the American Cancer Society
- Online Guide to Quitting
- Maryland Tobacco Quitline
- Affordable Care Act Tobacco Cessation Guidance Toolkit
- Familydoctor.org patient education articles
- Electronic Nicotine Delivery Systems (ENDS) Fact Sheet
- JUUL® Fact Sheet
Other Clinical Practice Tools
- Treating Tobacco Use and Dependence: Clinical Practice Guideline
- Quick Reference Guide for Clinicians
- Nicotine Replacement Therapy Medication List
- SmokeFree.Gov Partner Toolkit for Physicians
- AAFP Treating Tobacco Dependence Manual
Clinical Efficacy of Telemedicine & Audio-Only Encounters for Smoking Cessation
- Merianos, A. L., Fevrier, B., & Mahabee-Gittens, E. M. (2021). Telemedicine for Tobacco Cessation and Prevention to Combat COVID-19 Morbidity and Mortality in Rural Areas. Frontiers in public health, 8, 598905. doi.org/10.3389/fpubh.2020.598905.
- Kayhan Tetik, B., Gedik Tekinemre, I., & Taş, S. (2020). The Effect of the COVID-19 Pandemic on Smoking Cessation Success. Journal of community health, 1–5. Advance online publication. doi.org/10.1007/s10900-020-00880-2.
- Nomura A, Tanigawa T, Muto T, et al. Clinical efficacy of telemedicine compared to face-to-face clinic visits for smoking cessation: multicenter open-label randomized controlled noninferiority trial. J Med Internet Res. 2019;21(4):e13520. 4. DOI: 10.2196/13520
- Richter KP, Shireman TI, Ellerbeck EF, et al. Comparative and cost effectiveness of telemedicine versus telephone counseling for smoking cessation. J Med Internet Res. 2015;17(5):e113. DOI: 10.2196/jmir.3975
- Liebmann EP, Preacher KJ, Richter KP, et al. Identifying pathways to quitting smoking via telemedicine-delivered care. Health Psychol. 2019;38(7):638-647. DOI: 10.1037/hea0000740
- Barua RS, Rigotti NA, Benowitz NL, et al. 2018 ACC expert consensus decision pathway on tobacco cessation: a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2018;72(25):3332-3365. DOI: 10.1016/j.jacc.2018.10.027.
References
The following are references for this article where a complete citation was not embedded within the text.
Alcohol, Tobacco, Tax, and Trad Bureau. Data for Tobacco Statistical Release. Accessed: Apr 09 2021 from https://www.ttb.gov/tobacco/tobacco-statistics.
Ali FRM, Diaz MC, Vallone D, et al. E-cigarette Unit Sales, by Product and Flavor Type — United States, 2014–2020. MMWR Morb Mortal Wkly Rep 2020;69:1313–1318. DOI: http://dx.doi.org/10.15585/mmwr.mm6937e2.
National Center for Health Statistics. Percentage of current cigarette smoking for adults aged 18 and over, United States, 2019 Q1, Jan-Mar—2020 Q2, Apr-Jun. National Health Interview Survey. Generated interactively: Apr 09 2021 from https://wwwn.cdc.gov/NHISDataQueryTool/ER_Quarterly/index_quarterly.html.
National Center for Health Statistics. Percentage of current electronic cigarette use for adults aged 18 and over, United States, 2019 Q1, Jan-Mar—2020 Q2, Apr-Jun. National Health Interview Survey. Generated interactively: Apr 09 2021 from https://wwwn.cdc.gov/NHISDataQueryTool/ER_Quarterly/index_quarterly.html.
National Center for Health Statistics. Percentage of current cigarette smoking for adults aged 18 and over, United States, 2019, Jan-Jun—2020, Jan-Jun. National Health Interview Survey. Generated interactively: Apr 09 2021 from https://wwwn.cdc.gov/NHISDataQueryTool/ER_Biannual/index_biannual.html
National Center for Health Statistics. Percentage of current electronic cigarette use for adults aged 18 and over, United States, 2019, Jan-Jun—2020, Jan-Jun. National Health Interview Survey. Generated interactively: Apr 09 2021 from https://wwwn.cdc.gov/NHISDataQueryTool/ER_Biannual/index_biannual.html
North American Quitline Consortium. Report on the Impact of the COVID-19 Pandemic on Smoking Cessation. (Editors: L. Bailey and K. Mason). March 2021. Phoenix, AZ. cdn.ymaws.com/www.naquitline.org/resource/resmgr/reports-naqc/report_impact__of_covid-19_p.pdf.
Philip Gendall, PhD, Janet Hoek, PhD, James Stanley, PhD, Mathew Jenkins, PhD, Susanna Every-Palmer, PhD, Changes in Tobacco Use During the 2020 COVID-19 Lockdown in New Zealand, Nicotine & Tobacco Research, 2021; ntaa257. doi.org/10.1093/ntr/ntaa257.
Stämpfli, M., Anderson, G. How cigarette smoke skews immune responses to promote infection, lung disease and cancer. Nat Rev Immunol 9, 377–384 (2009). doi.org/10.1038/nri2530.